 🖨️ Print post
🖨️ Print post
A teratogen is a substance that causes malformation of a fetus, including birth defects and death. Teratogens also cause harm to the prenatal brain, affecting future intellectual, behavioral and emotional development and functioning. Exposures to teratogenic substances result in a wide variety of defects that range from infertility, prenatal onset growth restriction, structural defects and functional central nervous system (CNS) abnormalities to miscarriage or fetal death.1
Exposures in pregnancy can affect the fetus as early as ten to fourteen days after conception. During development, certain organs form at specific times but some structures are sensitive to teratogens throughout the entire pregnancy. Extremely serious defects of the brain and spine, called collectively neural tube defects (NTDs), occur in the first three to five weeks. NTDs include anencephaly (partial skull), spina bifida (opening in the spinal column) and other conditions affecting the brain, spine or neck.2
Many commonly used substances like ethanol (alcoholic beverages), herbicides and even saunas can cause birth defects. Viral infections, radiation, drugs, maternal disease or metabolic conditions (diabetes, hypothyroid), heavy metals in the environment, malnutrition or nutrient deficiencies and goitrogens can also be major factors.3
Mercury (Hg) is a major teratogen, considered one of the most toxic substances on earth and a serious global pollutant. Natural emissions of mercury into the air and water occur from volcanic eruptions, through weathering of rocks, degassing of the earth’s crust and evaporation of water. Man-made sources of mercury include industrial pollution, burning fossil fuels (the largest source of pollution), mining (gold, silver), refuse incineration, cremation and factory production. Mercury is no longer mined in the U.S.—most mercury today comes from mines in Spain, China, Kyrgyzstan and Algeria. Mercury is often used in gold mining, and many small operators in Africa use children to separate out the gold. Paints and building materials such as roofing shingles contain mercury, which can be released during use and disposal. Fossil fuel-burning power plants are the largest source of mercury pollution.4
Researchers have positively identified various teratogens through observation, anecdotal evidence, animal studies and examination of human exposures. Studies on animals have found mercury to be extremely cytotoxic, neurotoxic, immunotoxic and genotoxic; it is also an endocrine disrupter and a cause of infertility and fertility problems. These toxic effects have been documented by the U.S. Department of Health and Human Services’ Agency for Toxic Substances and Disease Registry (ATSDR). The extreme toxicity of mercury can be seen from documented effects on wildlife at very low levels of exposure. Because of its extreme toxicity, only one-half gram of mercury is required to contaminate the ecosystem and fish of a ten-acre lake to the extent that a health warning would be issued by the government not to eat the fish.5
Mercury is one of the most insidious and dangerous teratogens on earth because it has ready access to the human body even before birth, while the baby is in utero. The unborn are most at risk from the effects of mercury. It can be inhaled, passed through the skin or ingested. Mercury exposure even once during a pregnancy can cause harm to the unborn child’s body and mind, while continued exposure causes increasingly serious defects.5
FISH CONSUMPTION
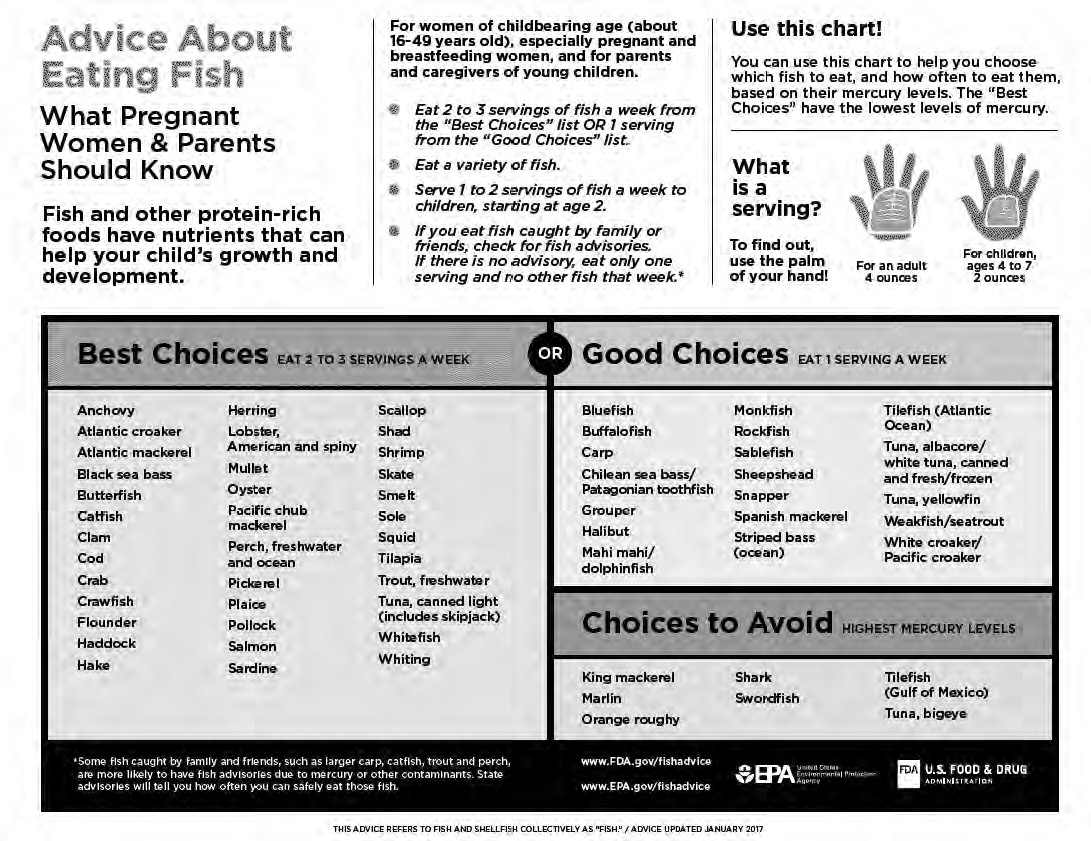
The Food and Drug Administration (FDA) and Environmental Protection Agency (EPA) recommend that women who are pregnant, breastfeeding or plan on becoming pregnant; women of childbearing age; and children consume more fish—two to three servings (eight to twelve ounces) from the “Best Choices” list or one serving from the “Good Choices”—but avoid seven specific fish highest in mercury. They say that children should eat one to two seafood meals per week starting at age two. The 2017 FDA chart “Advice about Eating Fish” (below) provides more detailed information,11 but this advice does not appear to differ much from the 2004 advisory, which recommended up to twelve ounces of fish per week and avoidance of specific fish high in mercury.12

The Centers for Disease Control and Prevention (CDC) have this to say about pregnant women and fish consumption: “Most fish purchased in the market in the United States do not have mercury levels that pose a risk to anyone, including pregnant women. Since mercury accumulates in the muscles of fish, larger fish that feed on smaller fish and live for long periods usually have larger concentrations of methylmercury (MeHg) than fish that feed on plants. For example, shark and swordfish normally contain the highest levels of mercury out of all ocean fish. Scientists have an ongoing debate about the value of fish in the diet versus any risk from increased exposure of pregnant women to methylmercury that may be in the fish. The safety of most fish sold commercially in the United States is regulated by the FDA. These fish pose no health risks to those who eat them. Only fish or wildlife containing relatively high levels of methylmercury are of concern.”13
Although most wild-caught fish are good nutritional choices, wild-caught fatty fish, such as salmon, sardines and anchovies, are the best choices because they contain more of the important omega-3 fatty acids. Fish, often called “brain food,” contain important amounts of the omega-3 fatty acids EPA and DHA, which are important for proper fetal development, including neuronal, retinal and immune function. DHA is especially important for brain and eye development. Fish are also an excellent source of fat-soluble vitamins like A, D, E and K. Oysters are an excellent source of zinc and are on the FDA “Best Choices” list.11
In addition, wild-caught fish contain antioxidants. Marine fish (but not fresh water fish) carry their own detoxification agent in the form of selenium, a powerful detoxifying agent known to detox mercury. Yellowfin, mahi mahi, skipjack, spearfish, wahoo, albacore, bigeye, and monchong contain high amounts of selenium.14 Other good sources of selenium are organ meats, such as chicken livers and gizzards, and brazil nuts. Experiments show that selenium-treated animals may remain unaffected, even when they have attained tissue mercury levels otherwise associated with toxic effects.15
Tuna protects itself by taking in an atom of selenium for every mercury atom. Indeed, one paper shows that with increasing levels of mercury, selenium levels also increased.15 In one unique study, a researcher compared an analysis of tuna from the nineteenth century that was preserved in a museum display case with a sample from 2002. Both samples showed about the same levels of mercury, as well as protective levels of selenium.16
According to the FDA, fish that should be avoided are tilefish, swordfish, orange roughy, marlin and king mackerel.11 Fish from local waters should be first investigated with the local fish commission before serving them for dinner.13
The idea that maternal fish consumption can reduce IQ in the child and cause neurological consequences is a contentious subject. As already mentioned, fish are a powerhouse of nutrients, including being good sources of DHA. The levels of DHA in the breast milk of American women are some of the lowest in the world.17-19 Restricting fish in the diet lowers the DHA levels even more, as do the high levels of omega-6 fatty acids that have pervaded the food system over the last century, because diets high in omega-6 inhibit conversion to DHA of alpha linolenic acid (ALA)20 (the short-chain omega-3 fatty acid found in plant foods like flax and walnut).
As fish is a source of methylmercury, however, fish is a cause for concern for families and public health officials. When mercury is released into the oceans, it is taken up by fish, shellfish and sea mammals, who transform it by methylation into methylmercury. Larger fish contain more methylmercury; whale blubber and muscle meat, consumed by certain populations, contain the highest levels of mercury contamination.21
There have been downward shifts in children’s IQ in the last century22 and some authorities think the decline is related to mercury in food.23 However, some fish-eating societies produce children with higher IQs. The average national IQ is highest in Hong Kong, followed by Singapore, South Korea, Japan, China, Taiwan, Italy, Iceland and other Scandinavian countries. In most of these countries people eat a lot of fish. These figures came from the work of Richard Lynn, a British professor of psychology, and Tatu Vanhanen, a Finnish professor of political science, who conducted studies in eighty countries. They concluded that IQ differences relate to national income, inequality, poverty, education quality and other factors.24 According to the IQ society Mensa International, Finland, Sweden and the U.K., have the most geniuses per capita. All are big fish-eating countries.
The Japanese continue to eat whale and dolphin meat, which can be purchased in the grocery store. In 2003, packaged whale meat steaks in grocery stores in Japan tested dangerously high in levels of mercury.26 In 2010 American scientists who sampled one thousand sperm whales were stunned at the high levels of toxins and heavy metals in the animals, which they called “jaw dropping.”27 These included mercury, aluminum, lead, silver, titanium and chromium, mostly in the blubber. A recent study found samples of dried pilot whale meat purchased in Japan contained 19 ppm mercury, 47.5 times over the legal limit. Dolphin meat contained 11 ppm.28
In contrast, albacore tuna sold in the U.S. contains an average of .32 ppm of mercury while light tuna has .12 ppm.29 However, results of a study done by the Mercury Policy Project, published in the report, “Tuna Surprise,” found that mercury levels in light and white tuna from government-sponsored school lunch programs had mercury levels four times the average reported by the FDA.30
MERCURY IN PROCESSED FOOD
In 2009, The Washington Post reported that “Almost half of tested samples of commercial high fructose corn syrup (HFCS) contained mercury, which was also found in nearly a third of 55 popular brand-name food and beverage products where HFCS is the first- or second-highest labeled ingredient, according to two new U.S. studies.”
HFCS has been extensively used in the U.S. food chain from 1970 to the present. Carbonated beverages (soda), very popular with children and adolescents, contain very high quantities of HFCS but its presence is universal in almost all food products, even bread. On average, Americans consume twelve teaspoons of HFCS per day, but teens can consume 80 percent more than average. Starting in the 2000s, the food manufacturers began to remove HFCS from food products due to consumer education efforts and choices, but it is still very much apparent in the food chain, especially in fast foods favored by children and foods served to children in school lunches. In 2009, four factories in the U.S. were still using technology that used mercury to produce the product. HFCS’s presence is still relatively unnoticed in condiments, such as mustards and ketchup, and in cheaper varieties of jams and other sweetened products.32
Protein powders are popular with teens and young adults, as well as bodybuilders of all ages. Young women are especially fond of protein powders in shakes and smoothies. Yet these health-conscious groups are perhaps not aware that they are contaminating their bodies with heavy metals every time they sip their protein shake.
The Clean Label Project recently completed a study of one hundred thirty-four protein powders from fifty-two brands at a third-party testing lab, which screened for toxins like mercury and other heavy metals, pesticides and other contaminants associated with cancer and other diseases. Over 70 percent of the protein powders had detectable levels of lead, and 74 percent showed cadmium. In addition to lead and cadmium, the powders contained varying levels of mercury and arsenic.
Overall, products from plant protein such as soy or hemp contained twice as much lead and high amounts of other contaminants, which could be due to plants absorbing heavy metals from the soil.33-34 In 2010, Consumer Reports published a report about the heavy metals they found in protein powder.
The Clean Label website does not give an explanation of their five-star rating and how they assigned a score for each product for four elements: heavy metals, pesticides, contaminants and nutrition. They only mention that the heavy metal content accounted for over 60 percent of the score.36
In 2017, the same company tested almost five hundred infant formula and baby food products for heavy metals and contaminants and found that over 30 percent of these products contained lead, arsenic, mercury, pesticides and acrylamides. Soy formulas contained seven times more cadmium than other formulas.
Another big source of heavy metals in the food chain is rice, containing high levels of mercury and arsenic. Rice-based infant cereal can be contaminated by mercury leaching into soil. In the U.S., Consumer Reports tested domestic rice and found high levels of arsenic.38
Rice baby cereal is the most common first food, which is introduced to the infant between four and six months of age. In a 2017 study in The Journal of Food Chemistry, researchers reported results from testing one hundred nineteen infant cereals sold in the U.S. and China and estimated the total mercury (THg) and methylmercury levels. Rice-based cereals contained methylmercury levels significantly higher than those of non-rice cereals. They concluded that cereal consumption could be a potential pathway for methylmercury exposure in infants.39
Another 2017 study, from the University of South Carolina, measured methylmercury and inorganic arsenic in thirty-six baby rice cereals, eight teething biscuits and four baby cereals made with oats or wheat. Rice cereals and teething biscuits were 61-92 times higher in methylmercury and higher in total arsenic, compared to wheat or oat baby cereals.40
Seed grains are treated with methylmercury to kill fungus and were the source of contaminated wheat and barley that caused a major mercury poisoning in Iraq in 1971. The seeds were imported from the U.S. and Mexico. People suffered major neurological consequences including numbness, lack of coordination and blindness. Around four hundred sixty people reportedly died. It was the largest mercury poisoning up to that time.41
MERCURY IN BREAST MILK
Inorganic mercury and methylmercury can pass from a mother’s body into breast milk and into a nursing infant. The amount of mercury in the milk will vary, depending on the degree of exposure and the amount of mercury that enters the nursing woman’s body. There are significant benefits to breastfeeding, so any concern that a nursing woman may have about mercury levels in her breast milk should be discussed with her doctor. Methylmercury can also accumulate in an unborn baby’s blood at concentrations higher than the concentration in the mother.42
A 2002 study showed that levels of mercury and lead (Pb) in breast milk concentrations are low. The authors concluded that “even theoretical risks from current mercury or lead levels for the breastfed infant of a healthy mother [could] be ruled out.”43
MERCURY IN MEDICINE AND DENTISTRY
In a 1961 medical text, Dr. Ernst Baader reported that the term “quack,” used to describe a person who pretends to have medical knowledge, originated from the German word Quecksalver―an individual who uses mercury ointments to treat disease.
Medicine is no stranger to the use of mercury, and children’s and women’s complaints were often the target. Calomel (mercury chloride) was once universally given to teething infants. Mercury was used in medications for women for “hysteria.” Decades and generations of patients were subjected to constant exposure to mercury from medicines, a practice that has continued unabated to the present in one form or another.
Josef Wakany, MD, a teratogen expert, lamented the issue of mercury poisoning in his paper on acrodynia, or “pink disease,” which was rampant between 1920 and 1950, but appeared earlier in Australia, the U.K. and worldwide. It killed, maimed and deformed many children. The disease was created by administering mercury to infants and children in teething powders, de-wormers and laxatives used for constipation, diarrhea and other conditions. Dr. Wakany said that physicians of the nineteenth century were familiar with symptoms of mercury poisoning and would have diagnosed mercury poisoning “at a glance.” However, physicians of the twentieth century were slow to recognize that the symptoms of acrodynia were caused by mercury, and many children were harmed unnecessarily. Products containing mercury were not removed from shops and pharmacies until the 1950s. Even then, physicians debated the premise that mercury was to blame.45
In addition to numerous physical symptoms, children also experienced psychiatric symptoms such as depression and melancholy. Physicians in 1946 described a depressive syndrome among children in a nursery (five to eleven months of age). Several of the children died and arrested development was noted in others. The doctors considered the illness comparable to melancholia in the adult and caused by “withdrawal of the love object.” The psychic diagnosis was outwardly rejected by physicians who attributed the depression to acrodynia.46
Dr. Ernst Baader reported many psychiatric symptoms of mercury poisoning, such as anxious seclusion, shyness, labile moods, forgetfulness, memory loss, feelings of intellectual inadequacy, fatigue, sleep disturbance, tremor, jerks, shaky handwriting, difficulty speaking, headaches, pressure over the head and sensory skin disturbances likened to crawling insects. These were often misdiagnosed as hysteria, schizophrenia or general emotional disturbance. These symptoms are similar to today’s common psychiatric conditions.46
In acrodynia, demyelination and degeneration of the insulative lipid sheath surrounding the nerve, also observed in multiple sclerosis (MS), was noted in biopsies of the time. Also noted were disturbances of blood circulation and temperature regulation; in severe cases fingers and toes could be lost by gangrene. Blood pressure and levels of the “stress hormone” adrenaline were often high. The victims exhibited extreme muscle weakness; they usually couldn’t stand or walk. Loss of weight, tremor and shaking, cramps and uncontrolled movements, abdominal tenderness and gastrointestinal troubles belonged to the clinical picture. Conjunctivitis and fever were also reported in earlier descriptions. Fever was apparently very common in Germany and Switzerland, where the most common misdiagnosis was scarlet fever. In a considerable number of cases, there was excessive salivation, swollen gingiva, loss of teeth and necrosis of the jaws. All these signs and symptoms can be attributed to mercury poisoning.46
Concurrently with doctors prescribing calomel in medicines and salves, dentists were putting another source of mercury into the mouths of children in the form of mercury amalgams, also called “silver” fillings, which are 50 percent mercury. In fact, the first dental amalgam was placed in 1830 in the U.S. Dental amalgams are still being used and are the filling of choice for poorer children on the Medicaid program. The American Dental Association continues to endorse amalgam fillings as “safe, affordable and durable.”47
Proposition 65, passed by the state of California in 1986, lists mercury as a reproductive toxin and a cause of birth defects. Thus, in California products that use mercury and cause significant mercury exposure must provide warnings to the public of the known health risk. Use of dental amalgam by dentists in California requires such a warning. Several other states have passed similar laws requiring warnings by dentists about the known health risks related to use of dental amalgam. Dental amalgam has been documented by tests at medical labs to be the largest source of mercury exposure for most people who have several amalgam fillings, with exposure levels as much as ten times the average for those without amalgam fillings.48
Dental amalgam in pregnant mothers is the largest source of mercury to the fetus and young infants.49 It readily crosses the placenta and also the blood-brain barrier.50 In order to minimize the chances of autism, developmental disability, lower IQ and physical defects, women of reproductive age and those contemplating pregnancy would be well advised to have their mercury amalgams removed by a dentist who is trained in such procedures as soon as possible before pregnancy occurs.
In the late 1940s, when the mercury etiology of acrodynia was clarified, the possibility of multiple sclerosis (MS) as an adult form of acrodynia was also considered. No general and widespead source of mercury was then recognized. However, in 1966, Baasch, a Swiss neurologist, recognized the possibility of amalgam fillings being such a source. He concluded that a mercury amalgam etiology could explain the known facts about MS and that additional protective or aggravating factors in the environment could play a role. Lead was also considered as a possible contributing factor because of its widespread occurrence, known demyelinating activity and some reports of MS after lead exposure.46
After calomel was removed from use, another source of mercury took its place. Thimerosal (ethylmercury) was first used in vaccines in the 1930s and the amounts increased beginning in 1989, with a sharp rise in 1990 as new vaccines were added to the schedule. This increase closely coincided with a dramatic increase in autism spectrum disorder (now at one in thirty-six children), a rise in attention deficit disorder, and a steady rise in the prevalence of developmental disability.9
Before 1989, the maximal dose of thimerosal by age two was 200 micrograms (mcg) but by the 1990s, it rose to 237.5 mcg. In the early 2000s, companies started to remove thimerosal from the vaccines. However, it is still present in the flu vaccine, which the CDC recommends to pregnant women and children over six months of age. The dangers of thimerosal were dismissed by experts who claimed that ethylmercury is quickly removed from the body. Studies show that it quickly clears the blood but is not excreted from the body. Instead it is deposited in organs and tissues, including the brain.
Thimerosal is used as a preservative in multi-dose vials of vaccine. If single-dose vials were normally in use, it would not be necessary. In 1999 when two pharmaceutical companies offered to supply thimerosal-free vaccines, the CDC rejected this offer and allowed the vaccine industry to sell its existing stocks which were not exhausted until 2003.9
That mercury can affect fertility is well known since mercury was commonly used as a spermicide in birth control products.51 Potential effects can be seen from effects on wildlife. Some Florida panthers that eat birds and animals that eat fish, frogs and turtles containing very low levels of mercury (about one part per million) have died from chronic mercury poisoning. Since mercury is an estrogenic chemical and a reproductive toxin, the majority of the remaining panthers cannot reproduce. The average male Florida panther has estrogen levels as high as females due to the estrogenic properties of mercury.52
WHY IS MERCURY SO DEADLY?
Mercury severely affects humans because this heavy metal has diffuse and widespread adverse effects on the human metabolism.
A wide distribution of sulfhydryl (SH) groups (organosulfur compounds) abounds in the human body. Methylmercury has a high affinity for sulfhydryl groups of amino acids, which are the building blocks for enzymes. As a pro-oxidant, mercury functions as a catalyst and oxidizes such groups. As with fluoride, mercury interferes with the formation and function of many proteins and enzymes by combining with them. It also disrupts protein synthesis, which is potentially the major cause of neurotoxicity. It also causes chromosomal breaks and DNA damage. Mercury is a radiomimetic metal with the same effects on the chromosomes and body systems as radiation.
Methylmercury is readily absorbed into the GI tract after ingestion, and 90 percent can be found in red blood cells bound to hemoglobin.
Mercury in low concentrations in cellular and animal experiments produces serious disturbances in basal metabolic processes, disrupting microtubules in the neuronal cytoskeleton. It binds to thiols in the tubulin and blocks the electric activity in microtubules, which are required for many cellular functions, including division and migration. It also affects the calcium balance in the microtubule.
The critical organ for methylmercury toxicity is the brain. Mercury causes damage throughout the brain. The target organs for elemental mercury are the brain and kidney. It readily crosses the blood-brain barrier and firmly binds to molecules in the brain. There is no innate mechanism for rapid removal.50
Astrocytes in the brain have a special role in early brain development and methylmercury inhibits these functions. Methylmercury preferentially accumulates in astrocytes, which make up about 50 percent of the CNS volume and perform many important duties. They prevent leaky blood-brain barrier, which limits the transport of toxins into the brain and allows nutrients to pass. Astrocyte dysfunction is a main cause of neurotoxicity. Methylmercury inhibits glutamate uptake in astrocytes. It promotes and enhances free radical formation, which is known to play an important role in Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis (ALS). It activates specific signaling molecules, which leads to induction of genes that contribute to cell damage.
Brains of infants and animals exposed in utero show cell loss, reduced brain size, decreased protein production and changesin neurotransmission resulting in cerebral palsy and mental retardation.53
Retention is around 95 percent of intake for methylmercury, 80 percent for elemental mercury vapor, and 7 percent for inorganic mercury compounds. The toxicology of the three species of mercury intertwine because organic mercury and elemental mercury convert to inorganic mercury in the brain. The dose in the brain from dental amalgams and methylmercury may be cumulative. Inorganic mercury can remain in the brain for years. Daily excretion of methylmercury through the bile and feces is about 1 percent of the body burden.50
Mercury depletes antioxidants such as selenium, which are needed for thyroid function, building selenoproteins and many other processes. Selenium depletion, as well as zinc depletion, influences neuronal function and produces defects in neuronal plasticity, which can ultimately affect behavior in children with attention-deficit/hyperactivity disorder.54
PREVENTION
In the past, children were major targets of mercury poisoning through teething powders, laxatives, de-wormers, Mercurochrome, creams and salves. Today they are exposed to mercury in vaccines and dental amalgams, in addition to mercury in the air, water, soil, food, medicines, paint, cement, building materials, thermostats, thermometers, fungicides, light bulbs and other sources at home and at school. Some traditional Chinese and Hispanic remedies for stomach disorders contain mercury.
Parents should learn about sources of mercury and avoid bringing them into the home. Prevention and education are key to improving children’s health by reducing mercury exposure. By breastfeeding and avoiding infant formulas, the infant will ingest a lower amount of many toxins, including mercury. If breastfeeding is not possible, homemade infant formulas are a superior choice to any commercial formula. Babies, toddlers and young children typically consume high amounts of cereals, teething biscuits and other items made from rice, which contain mercury and other heavy metals. Traditionally, first foods for babies were liver and egg yolks. These continue to be outstanding sources of nutrients for young children. Adolescents and young adults who use protein powders daily or even occasionally compromise their immune system and systemic health through ingestion of heavy metals. Consuming carbonated sodas and other beverages and foods containing HFCS adds further to the body mercury burden. Children’s lunches and school events often feature food items that contain rice, HFCS or high sugar content, artificial color and flavorings, additives, maltodextrin and other sources of toxins.
Pediatricians, nurses, dentists and other health care providers must learn and understand the scope of mercury exposures and health problems among children and be prepared to handle mercury exposures in medical practice. Children, in contrast to adults, are the recipients of major sources of mercury through vaccines and dental amalgams. No “safe” level can protect the most vulnerable from mercury’s toxic effects.
SIDEBARS
FORMS AND SOURCES OF MERCURY
Mercury is a heavy metal that occurs in several basic forms: organic methylmercury (MeHg) and ethylmercury (EtHg), and inorganic (metallic or elemental) mercury. Organic mercury is the most dangerous form of mercury to human health.6
Historically, most of the research and concern regarding mercury’s toxic effects on humans and in particular on fetal development has focused on MeHg, which is considered one of the six most dangerous chemicals in the environment.7 MeHg can easily cross into the brain and body organs and is also extremely neurotoxic, much more so than inorganic forms. MeHg is better absorbed and shows a higher mobility in the human body than inorganic mercury. Ethylmercury is present in thiomersal, which has been used as a major preservative in vaccines.8 Today it is still in use in the flu vaccines recommended for pregnant women and children older than six months of age.9
MeHg is found mainly through food, especially fish ingestion, although industrial pollution is also a dangerous source. Mass poisonings affected many in Iraq when people consumed bread made from seeds sprayed with mercury. There have been highly publicized major acute poisonings affecting many people and infants exposed through eating fish in Japan at Minamata Bay in 1956. The Minamata disaster was caused by release of MeHg into the bay by the Chisso Chemical Corporation.10
REFERENCES
1. Teratogens. Children’s Hospital of Wisconsin. http://bit.ly/2n5Ram6.
2. Neural tube defects (NTDs): condition information. National Institute of Child Health and Human Development. http://bit.ly/2FkkTCW.
3. Gilbert-Barness E. Teratogenic causes of malformations. Ann Clin Lab Sci 2010;40(2):99-114.
4. Bose-O’Reilly S, McCarty KM, Steckling N, Lettmeier B. Mercury exposure and children’s health. Curr Probl Pediatr Adolesc Health Care 2010;40(8):186–215.
5. Bose-O’Reilly et al., 2010.
6. Hong YS, Kim YM, Lee KE. Methylmercury exposure and health effects. J Prev Med Public Health 2012;45(6):353–363.
7. Gilbert-Barness, 2010.
8. Bose-O’Reilly et al., 2010.
9. Kennedy RF, Jr. Thimerosal: Let the Science Speak. New York, NY: Skyhorse Publishing; 2014.
10. Bose-O’Reilly et al., 2010.
11. Eating fish: what pregnant women and parents should know. U.S. Food and Drug Administration (FDA). http://bit.ly/2BBh5Hc; 2017 EPA-FDA advice about eating fish and shellfish. Environmental Protection Agency (EPA). http://bit.ly/2H4HPTW.
12. What you need to know about mercury in fish and shellfish. EPA. http://bit.ly/2FhIqB4.
13. Agency for Toxic Substances & Disease Registry (ATSDR). Public health statement for mercury. March 1999. https://www.atsdr.cdc.gov/PHS/PHS.asp?id=112&tid=24.
14. Ralston NV, Raymond LJ. Dietary selenium’s protective effects against methylmercury toxicity. Toxicology 2010;278(1):112-23; Western Pacific Regional Fishery Management Council. Selenium in ocean fish protects against mercury. http://www.wpcouncil.org/wpcontent/uploads/2013/04/Selenium_Poster_final.pdf.
15. Skerfving S. Interaction between selenium and methylmercury. Environ Health Perspect 1978;25:57-65.
16. Emsley J. “Selenium.” Pp. 379-384 in: Nature’s Building Blocks: An A-Z Guide to the Elements. Oxford University Press; 2001.
17. Juber BA, Jackson KH, Johnson KB et al. Breast milk DHA levels may increase after informing women: a community-based cohort study from South Dakota USA. Int Breastfeed J 2017;12:7.
18. Brenna JT, Varamini B, Jensen RG et al. Docosahexaenoic and arachidonic acid concentrations in human breast milk worldwide. Am J Clin Nutr 2007;85(6):1457-1464.
19. Stark KD, Van Elswyk ME, Higgins MR et al. Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog Lipid Res 2016;63:132-152.
20. Gibson RA, Neumann MA, Lien EL et al. Docosahexaenoic acid synthesis from alphalinolenic acid is inhibited by diets high in polyunsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids 2013;88(1):139-146.
21. “Jaw-dropping” levels of heavy metals found in whales. Boston.com, June 25, 2010. http://bit.ly/2oPizcD.
22. Breslau N, Chilcoat HD, Susser ES et al. Stability and change in children’s intelligence quotient scores: a comparison of two socioeconomically disparate communities. Am J Epidemiol 2001;154(8):711-717.
23. Schwartz J. Mercury from fish does not reduce children’s IQs. Environ Health Perspect 2006;114(7):A399–A400.
24. World ranking of countries by their average IQ. IQ Research. http://bit.ly/1O7VYBV.
25. Dicker R. These are the world’s 10 smartest countries. U.S. News, Sept. 2, 2016. http://bit.ly/2Ftl4M2.
26. Graham S. Packaged whale meat in Japan contain high levels of mercury. Scientific American, May 20, 2003. http://bit.ly/2oQM0Lu.
27. “Jaw-dropping” levels of heavy metals found in whales. http://bit.ly/2oPizcD.
28. Kirby D. The Internet giant that is selling toxic whale and dolphin meat in Japan. Takepart.com, Apr. 8, 2015. http://bit.ly/1Oek4XB).
29. Mercury alert: is canned tuna safe? Environmental Defense Fund. http://bit.ly/2Fs3Pe9.
30. Groth E. Tuna surprise: mercury in school lunches. Montpelier, VT: Mercury Policy Project. http://mercurypolicy.org/wpcontent/uploads/2012/09/mpp_tuna_surprise_final_final1.pdf.
31. Study finds high-fructose corn syrup contains mercury. Washington Post, Jan. 28, 2009. http://wapo.st/1HgvEMP.
32. Infertility, birth defects related to mercury from amalgam dental fillings. Dental Amalgam Mercury Solutions (DAMS). http://amalgam.org/377-2/.
33. Schultz H. Study that alleges that many protein powders contain heavy metals gets big pushback, including threatened legal action. NutraIngredients-USA. Mar. 2, 2018. http://bit.ly/2Fi2kiK.
34. Clean Label Project. 2018 protein powder study. http://www.cleanlabelproject.org/protein-powder/.
35. Health risks of protein drinks. You don’t need the extra protein or the heavy metals our tests found. Consumer Reports, July 2010. http://bit.ly/2zESmWx.
36. Hirsch J. Arsenic, lead found in popular protein supplements. Consumer Reports, Mar. 12, 2018. http://bit.ly/2F51Dtu.
37. Clean Label Project. Infant formula and baby food project summary. http://www.cleanlabelproject.org/infant-formula-baby-food/.
38. Arsenic in your food: our findings show a real need for federal standards for this toxin. Consumer Reports, Nov. 2012. http://bit.ly/S7suEy.
39. Cui W, Liu G, Bezerra M et al. Occurrence of methylmercury in rice-based infant cereals and estimation of daily dietary intake of methylmercury for infants. J Agric Food Chem 2017;65(44):9569-9578.
40. Rothenberg SE, Jackson BP, Carly McCalla G et al. Coexposure to methylmercury and inorganic arsenic in baby rice cereals and rice-containing teething biscuits. Environ Res 2017;159:639-647.
41. Bose-O’Reilly et al., 2010.
42. ATSDR, 1999.
43. Gundacker C, Pietsching B, Wittlmann KJ et al. Lead and mercury in breast milk. Pediatrics 2002;110(5):873-878.
44. Baader EW. “Quecksilbervergiftung” [“Mercury Poisoning”]. Pp. 158-176 in: Handbuch der Gesamten Arbeitsmedizin [Handbook of Occupational Medicine]. Munich: Urban and Schwarzenberg; 1961.
45. Warkany J. Acrodynia—postmortem of a disease. Am J Dis Child 1966;112(2):147-156.
46. Hanson M. A hundred and fifty years of misuse of mercury and dental amalgam. http://art-bin.com/art/hanson_en.html.
47. Statement on Dental Amalgam. American Dental Association (ADA). http://bit.ly/2FoJZQW.
48. Infertility, birth defects related to mercury from amalgam dental fillings. DAMS. http://amalgam.org/377-2/.
49. Palkovicova L, Ursinyova M, Masanova V et al. Maternal amalgam dental fillings as the source of mercury exposure in developing fetus and newborn. J Expo Sci Environ Epidemiol 2008;18(3):326-331.
50. National Research Council (NRC). Toxicological effects of methylmercury. Washington, DC: National Academy Press; 2000. ASTDR. Toxicological profile for mercury. U.S. Department of Health and Human Services, Mar. 1999. http://bit.ly/2CXVwl6.
51. Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments (Seventh Issue). New York: United Nations; 2002.
52. Facemire CF, Gross TS, Guillette LJ. Reproductive impairment in the Florida panther. Health Perspect 1995;103(4):79-86.
53. Aschner M, Syversen T, Souza DO et al. Involvement of glutamate and reactive oxygen species in methylmercury neurotoxicity. Braz J Med Biol Res 2007;40:285-291; Gilbert SG, Grant-Webster KS. Neurobehavioral effects of developmental methylmercury exposure. Environ Health Perspect 1995;103(Suppl 6):135-142.
54. Dufault R, Schnoll R, Lukiw WJ et al. Mercury exposure, nutritional deficiencies and metabolic disruptions may affect learning in children. Behav Brain Funct 2009;5:44.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly magazine of the Weston A. Price Foundation, Spring 2018.
🖨️ Print post

I work in the fitness industry, so my family and I eat a lot of fish in our diets. Thank you for sharing such great knowledge, Sylvia!