 🖨️ Print post
🖨️ Print post
FODMAPs are short-chain carbohydrates that some people have difficulty digesting. Research shows that a low-FODMAP elimination diet can be an effective diet for treating gastrointestinal symptoms associated with irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).1,2 The low-FODMAP diet also has been shown to reduce pain associated with fibromyalgia3 and increase quality of life for patients with chronic digestive conditions.1
Because of its effectiveness, the low-FODMAP diet is one of the most common diets we recommend at my clinic, the Ruscio Institute for Functional Medicine.
It’s important to note, however, that while the low-FODMAP diet can be a powerful therapy, it’s not intended to be a long-term solution. Rather, individuals can use the diet as a temporary tool to improve gut health and bacterial balance, after which point they can begin to reintroduce nutritious foods that were previously eliminated.
In this article, I’ll discuss the basics of the low-FODMAP diet, who can benefit from it and how to implement it simply and effectively. I’ll also provide guidance on what to do when transitioning off of the low-FODMAP diet and how to reintroduce healthy fermentable carbohydrates.
What is a FODMAP?
FODMAP stands for “fermentable oligosaccharides, disaccharides, monosaccharides and polyols.” In a nutshell, foods that fall into these categories are fermentable carbohydrates that can feed unhealthy bacteria in the gut. FODMAPs include fructose (in many fruits and vegetables), lactose (dairy products), fructans (in grains like wheat), glactans (in legumes) and sugar alcohols like xylitol and sorbitol.
For those whose gut ecology may have imbalances or overgrowths, high-FODMAP foods can escalate gut problems, triggering more inflammation and worsening symptoms. The low-FODMAP diet is an elimination diet meant to help individuals identify foods that trigger symptoms. By temporarily restricting consumption of high-FODMAP foods and then going through a gradual process of reintroduction, the individual can more clearly understand which specific foods are problematic and which can be safely consumed.
Essentially, the elimination period provides an opportunity for the gut to heal and for bacterial overgrowths or imbalances to be corrected.
While some people are highly sensitive to all types of FODMAPs and may need to stay on the full diet plan, most will be able to customize the diet to their needs. Simply lowering the overall consumption of FODMAP foods can help reduce the burden of symptoms. Knowing one’s unique trigger foods provides a sense of control over food reactions.
It is interesting to note that two of the foods most commonly connected with food reactions—gluten-containing grains and dairy foods—are both high-FODMAP foods. Researchers suggest that FODMAP sensitivity may be a factor in many cases of non-celiac gluten sensitivity.4,5
A Gut-Healing Diet
The majority of research into the low-FODMAP diet has focused on patients with IBS and IBD. Research shows significant benefits for patients with both conditions.2,6,7,8
It’s likely that the low-FODMAP diet is also beneficial for a wider range of gut conditions. That’s because with gastrointestinal disorders, labels can be tricky, and there is considerable overlap among conditions. For example:
- IBS and IBD may occur in the same patients.9
- Across fifty studies, more than one-third of IBS patients tested positive for small intestinal bacterial overgrowth (SIBO).10
- Some researchers categorize celiac disease, non-celiac gluten sensitivity and lactose intolerance among the umbrella category of IBS-like conditions.11
- IBS and IBD patients are more likely to have leaky gut (intestinal permeability).12
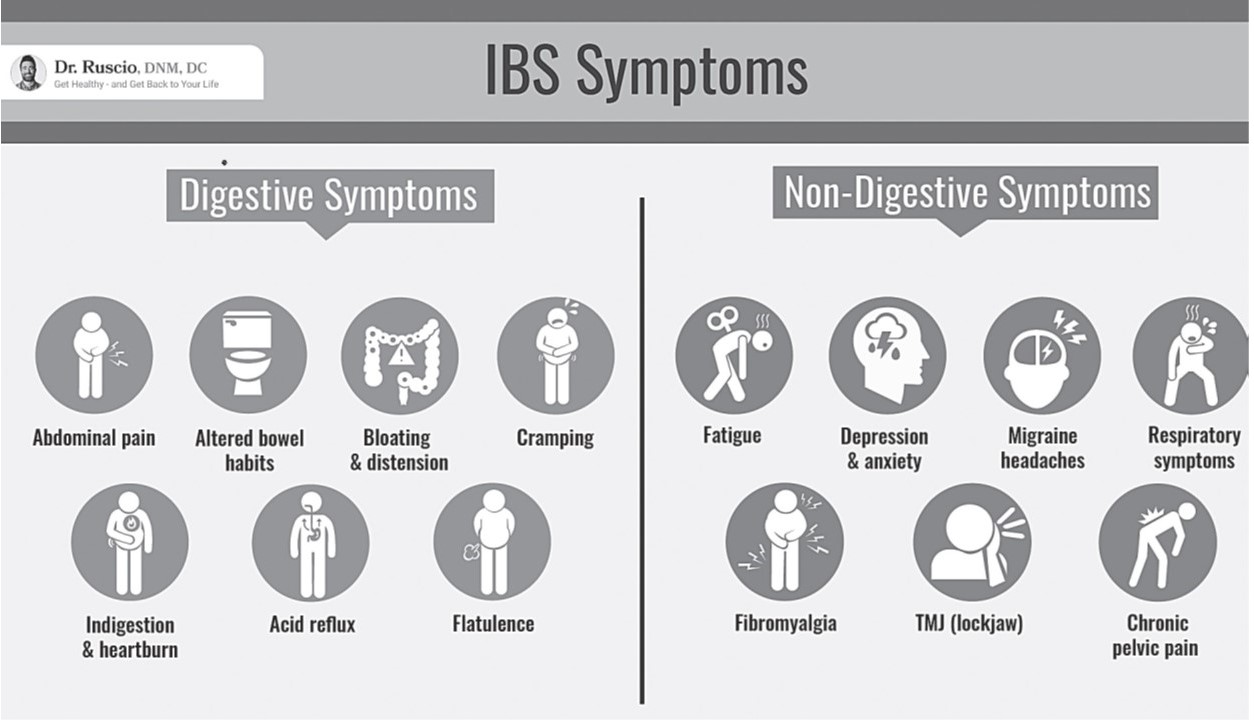
Furthermore, patients with IBS, IBD and other gut disorders share a surprising list of non-digestive symptoms, such as fatigue, headaches, anxiety, depression, joint pain, fibromyalgia and more (see Figure 1, previous page). Many of these “mystery symptoms” are the result of chronic inflammation, autoimmunity and even altered function of the central nervous system, which have their origin in poor gut health.13,14

For those with gut-related conditions and symptoms, the low-FODMAP diet is a proven option that individuals can safely explore without need for a formal diagnosis or medical supervision. We recommend a two- to three-week trial of the full diet to see whether FODMAP restriction results in symptom improvement.
An underlying factor behind most gut conditions and symptoms is gut dysbiosis—an imbalance between healthy and unhealthy microorganisms in the intestinal tract. Practitioners often compare an unhealthy gut ecosystem to a garden overgrown with weeds. Consuming high-FODMAP foods is much like adding fertilizer to a weed patch.
A low-FODMAP diet can result in significant improvements in the gut ecosystem, including reduction of bacterial overgrowths; less inflammation; healing of the gut lining; calming of overzealous immune responses; and better absorption of nutrients from food.
What the Research Shows
Two comprehensive meta-analyses (highest quality research evidence) determined that the low-FODMAP diet reduced overall digestive symptoms and abdominal pain, and increased the quality of life for patients with gastrointestinal disorders.12
Other research has shown that the low-FODMAP diet improved diarrhea in IBS-D;15 reduced digestive symptoms such as bloating, abdominal pain and gas;6,7,8,16,17,18 reduced leaky gut and gut inflammation;16,17 had a positive impact on gut endocrine cells, which can normalize bowel function;19,20,21 significantly improved histamine levels22 (although this finding has recently been challenged); and reduced pain for fibromyalgia patients.3
Another study indicated that the low-FODMAP diet works better than standard dietary advice.15 Research also suggests that the low-FODMAP diet may increase the amount of serotonin-producing cells in the intestines. Serotonin helps with reducing pain and with healthy motility (the movement of waste through the digestive tract).21 Finally, a randomized controlled trial found that the daily intake of most micronutrients for the low-FODMAP diet was stable and met the Recommended Dietary Allowances.23
The Low-FODMAP Diet in Practice
For most people, implementing a new dietary approach of any kind can feel overwhelming. My recommendation is to keep the diet as simple and basic as possible as one begins. Prior to starting, it is also important to have a good understanding of the foods to focus on and those to eliminate temporarily.
Table 1 summarizes the information I share with my patients when they prepare to start a low-FODMAP diet. The foods listed in the “safe” category are considered low-FODMAP and should constitute the bulk of what a person eats. Those listed under “caution” should be eaten sparingly and in small amounts. Those listed under “foods to avoid” should be eliminated as much as possible. Comprehensive FODMAP food lists can be found online and can be good resources to help get started.

At first glance, the low-FODMAP diet may seem counterintuitive because it eliminates a number of foods that are demonstrably nutritious. This is why it’s important to understand that a low-FODMAP diet is designed to be short-term. The foods one avoids on a low-FODMAP diet are not necessarily “bad”; they’re simply presenting a temporary challenge for the digestive system.
Combining the Low-FODMAP Diet with Traditional Food Principles
The low-FODMAP diet temporarily restricts certain foods that are staples of a Wise Traditions diet. For someone who has been following the Weston A. Price Foundation’s dietary guidelines, this might be confusing. However, when followed properly, a low-FODMAP protocol—an elimination period followed by reintroduction and maintenance phases—can actually set a person up to do even better with a Wise Traditions diet and traditional eating principles.
Remember, the purpose of a low-FODMAP diet is to improve digestive health. Once the low-FODMAP tool has helped someone to accomplish that goal, he or she will likely have an easier time digesting some of the more challenging (but nutritious) traditional foods like milk, meat and grains.
Low-FODMAP Diet Trial
There are three main phases of the diet:
- the elimination phase
- the reintroduction phase
- the maintenance phase
It may be helpful to track reactions or symptoms using a food journal.
The best way to know whether a low-FODMAP diet will work is to give it a two- to three-week trial. During this period, the desired outcome is a reduction in digestive symptoms and possibly non-digestive symptoms such as fatigue, headache and brain fog. Even minor symptom improvement should be considered an indicator of success. As a person continues with the diet, there will likely be more improvement as gut bacteria are rebalanced, inflammation subsides and the gut wall heals. If an individual does not experience any symptom improvement during the trial period, it’s likely the low-FODMAP diet does not work for that person. In this case, it is time to stop the diet and try something else.
Elimination Phase
During the elimination phase, the goal is to restrict consumption of high-FODMAP foods as much as possible. While doing the best one can, it’s important not to stress out about perfection.
After starting the elimination phase with a two- to three-week trial period, it’s time to assess whether there has been any symptom improvement. If there have been improvements, that is an indication to continue with the elimination phase. One can expect to see more symptom improvement as one continues with the elimination phase.
Reintroduction Phase
Once a person has hit a plateau of symptom improvement, he or she can start the reintroduction phase. The goal of this phase is to identify which FODMAP foods aggravate symptoms.
At this point, it’s helpful to be methodical in the reintroduction approach, starting by testing one serving of a high-FODMAP food (starting with the foods one misses most). After reintroduction, monitor for any type of reaction, waiting twenty-four to forty-eight hours because reactions to high-FODMAP foods may not be immediate.
Common reactions include gas, bloating, diarrhea or constipation. Reactions can also include non-digestive symptoms such as joint pain, brain fog, depression or anxiety. If a reaction occurs, continue to avoid that food. Allow a few days for the gut and immune system to calm down before reintroducing another food. If no reaction occurs, add that food back into the diet and move onto the next food.
Maintenance Phase
The final phase of the low-FODMAP diet is the maintenance phase. During this phase, the goal is to continue to broaden one’s diet while maintaining symptom remission. This phase is all about personalizing and customizing the low-FODMAP diet according to the results of the reintroduction phase.
Over time, individuals can continue to experiment with foods and refine what works best for them. It’s not uncommon for a high- FODMAP food to cause a reaction early on but be well tolerated months later as the digestive system heals. Focusing on listening to one’s body will help pinpoint the long-term dietary approach that works best.
I encourage patients to eat as broadly as possible while managing symptoms. I see many people who needlessly follow overly restricted diets and develop a fear of food. This is counterproductive and creates stress. It’s important to enjoy one’s food as much as possible and let it be part of the healing journey.
Enhancing Digestibility
During the reintroduction and maintenance phases, the goal is to broaden the diet as much as possible without triggering symptoms. This means increasing the intake of healthy, higher-FODMAP foods.
There are a number of things one can do to enhance the digestibility of food and increase tolerance during these phases, including continuing to choose foods that are whole, unprocessed and nutritious; choosing whole raw milk from pasture-fed cows, or fermented milk products like kefir; and consuming whole grains that have been soaked, sprouted or soured.
Probiotic Support
High-quality probiotic supplements are another safe, accessible and proven treatment that can make a significant difference in a healthy gut ecology. As with dietary changes, I recommend a two- to three-week trial; however, don’t do more than one trial at a time. It’s possible to start a trial of probiotics either before or after the low-FODMAP trial, monitoring symptoms. If any symptoms improve while taking probiotics, continue to take the probiotic supplement.
Worth a Try
For individuals experiencing gastrointestinal symptoms or struggling daily with a diagnosed condition like IBS or IBD, a temporary low-FODMAP diet can be a valuable tool. The low-FODMAP diet can help to manage symptoms, rebalance the gut ecology over time and improve quality of life. In combination, a low-FODMAP diet and quality probiotic supplements are effective, research-backed therapies that are safe and accessible to try at home. Although the diet and the probiotics should be trialed separately, together they can form the basis of a long-term strategy for better gut health.
SIDEBAR
Tips for Success on the Low-FODMAP Diet
KEEP IT SIMPLE. Making a dietary change can be overwhelming, but it doesn’t have to be. When beginning, choose a few staple foods and recipes. It’s okay to repeat meals when first starting. It will be easier to expand menu options and try new recipes once your food triggers have been identified.
PLAN AHEAD. Remove the high-FODMAP “foods to avoid” from the home and especially those that may be tempting to you. Stock the pantry and refrigerator with the foods you want to focus on eating. Create a simple low-FODMAP menu plan and use that to develop a standard grocery list. Batch-cook at the beginning of the week and store extra meals in the freezer.
BE AS STRICT AS POSSIBLE FOR TWO TO THREE WEEKS. During this time, follow the low-FODMAP diet as closely as possible. If the dietary changes are helpful, symptoms should improve during this time. Once symptoms have improved, you can slowly reintroduce one food at a time to identify your personal food triggers.
DON’T FEAR YOUR FOOD. As the digestive tract heals, the foods you can eat may change. You may find that you are able to eat moderate amounts of a food that previously caused a reaction. Don’t fall into the trap of thinking you will never be able to eat your trigger foods again. Aim for the fewest dietary restrictions as possible and develop a healthy, non-fear-based relationship with food.
REFERENCES
- Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016;55(3):897–906.
- Altobelli E, Del Negro V, Angeletti PM, et al. Low-FODMAP diet improves irritable bowel syndrome symptoms: a meta-analysis. Nutrients. 2017;9(9):940.
- Marum AP, Moreira C, Saraiva F, et al. A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients. Scand J Pain. 2016;13:166–172.
- Skodje GI, Sarna VK, Minelle IH, et al. Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterology. 2018;154(3):529-539.e2.
- De Giorgio R, Volta U, Gibson PR. Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction? Gut. 2016;65(1):169–178.
- Pedersen N, Ankersen DV, Felding M, et al. Low-FODMAP diet reduces irritable bowel symptoms in patients with inflammatory bowel disease. World J Gastroenterol. 2017;23(18):3356–3366.
- Zhan Y, Zhan Y-A, Dai S-X. Is a low FODMAP diet beneficial for patients with inflammatory bowel disease? A meta-analysis and systematic review. Clin Nutr. 2018;37(1):123–129.
- Gibson PR. Use of the low-FODMAP diet in inflammatory bowel disease. J Gastroenterol Hepatol. 2017;32 Suppl 1:40–42.
- Szałwińska P, Włodarczyk J, Spinelli A, et al. IBS–symptoms in IBD patients–manifestation of concomitant or different entities. J Clin Med. 2020;10(1):31.
- Chen B, Kim JJ-W, Zhang Y, et al. Prevalence and predictors of small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis. J Gastroenterol. 2018;53(7):807–818.
- Borghini R, Donato G, Alvaro D, et al. New insights in IBS-like disorders: Pandora’s box has been opened; a review. Gastroenterol Hepatol Bed Bench. 2017;10(2):79–89.
- Camilleri M, Madsen K, Spiller R, et al. Intestinal barrier function in health and gastrointestinal disease. Neurogastroenterol Motil. 2012;24(6):503–512.
- Takakura W, Pimentel M. Small intestinal bacterial overgrowth and irritable bowel syndrome – an update. Front Psychiatry. 2020;11:664.
- Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010;7(3):163–173.
- Zahedi MJ, Behrouz V, Azimi M. Low fermentable oligo-di-mono-saccharides and polyols diet versus general dietary advice in patients with diarrhea-predominant irritable bowel syndrome: a randomized controlled trial. J Gastroenterol Hepatol. 2018;33(6):1192–1199.
- Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: the FODMAP approach. J Gastroenterol Hepatol. 2010;25(2):252–258.
- Gibson PR, Shepherd SJ. Food choice as a key management strategy for functional gastrointestinal symptoms. Am J Gastroenterol. 2012;107(5):657–666; quiz 667.
- Cox SR, Lindsay JO, Fromentin S, et al. Effects of low FODMAP diet on symptoms, fecal microbiome, and markers of inflammation in patients with quiescent inflammatory bowel disease in a randomized trial. Gastroenterology. 2020;158(1):176-188.e7.
- Mazzawi T, El-Salhy M. Changes in duodenal enteroendocrine cells in patients with irritable bowel syndrome following dietary guidance. Exp Biol Med (Maywood). 2017;242(13):1355–1362.
- Mazzawi T, Hausken T, Gundersen D, et al. Dietary guidance normalizes large intestinal endocrine cell densities in patients with irritable bowel syndrome. Eur J Clin Nutr. 2016;70(2):175–181.
- Mazzawi T, El-Salhy M. Effect of diet and individual dietary guidance on gastrointestinal endocrine cells in patients with irritable bowel syndrome (Review). Int J Mol Med. 2017;40(4):943–952.
- McIntosh K, Reed DE, Schneider T, et al. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut. 2017;66(7):1241–1251.
- Eswaran S, Dolan RD, Ball SC, et al. The impact of a 4-week low-FODMAP and mNICE diet on nutrient intake in a sample of US adults with irritable bowel syndrome with diarrhea. J Acad Nutr Diet. 2020;120(4):641–649.
This article appeared in Wise Traditions in Food, Farming and the Healing Arts, the quarterly journal of the Weston A. Price Foundation, Winter 2021
🖨️ Print post

Has the FODMAP content of raw milk dairy been determined, such as raw cow’s milk, raw cow kefir, and colostrum?